The modern healthcare revenue cycle is defined by payer complexity. Each carrier enforces its own documentation requirements, medical necessity policies, denial rules, and audit triggers. That variability creates a compliance maze for hospitals and physician groups working with dozens of payers. What passes for one payer may be denied by another, and the financial stakes of navigating those differences are significant.
Most organizations still manage payer rules in silos: one team handles Medicare audits, another handles commercial denials, and others chase appeals from Medicaid MCOs. That fragmented approach loses valuable intelligence. Denials look like isolated events instead of cross-payer patterns that could be used to predict risk, negotiate contracts, and accelerate cash flow.
Cross-payer analytics changes that dynamic. By consolidating billing, coding, audit, and denial data and analyzing it across carriers, MDaudit enables leaders to uncover systemic drivers of denials, identify anomalies in payer behavior, and act before revenue is lost. Our approach in the Revenue Integrity Suite connects insights, action, and outcomes so teams can anticipate risk, fix it at the source, and measure impact.
Why Cross-Payer Visibility Matters
Denials are not distributed evenly across payers. Each carrier evolves its rules based on medical policies, utilization strategies, and contract terms. Without a cross-payer lens, organizations miss:
- Systemic patterns that affect many payers at once, such as diagnosis specificity gaps for infusion drugs.
- Outliers where one payer’s denial rates are significantly higher than peers for the same services.
- Shifting behavior as policies drift from one carrier to another, creating new risks if left undetected.
- Compliance exposure is driven by inconsistent documentation or coding practices across the enterprise.
A cross-payer view exposes these patterns so leaders can act at the enterprise level rather than fighting payer issues in isolation.
Questions Cross-Payer Analytics Should Answer Every Week
- Which denial reasons are increasing simultaneously across multiple payers—and which are isolated to a single policy?
- Where are MCC/CC combinations or DRG assignments drawing consistent downgrades regardless of payer?
- Which service lines or facilities show outlier denial rates with particular carriers compared to internal peers?
- Which providers or coders have payer-specific patterns that call for focused education or prospective review?
- How is payer mix shifting by location, and what does that imply for first-pass yield and cash?
When teams answer these questions continuously—not just in quarterly reviews—they stop fighting one-off fires and start solving repeatable problems.
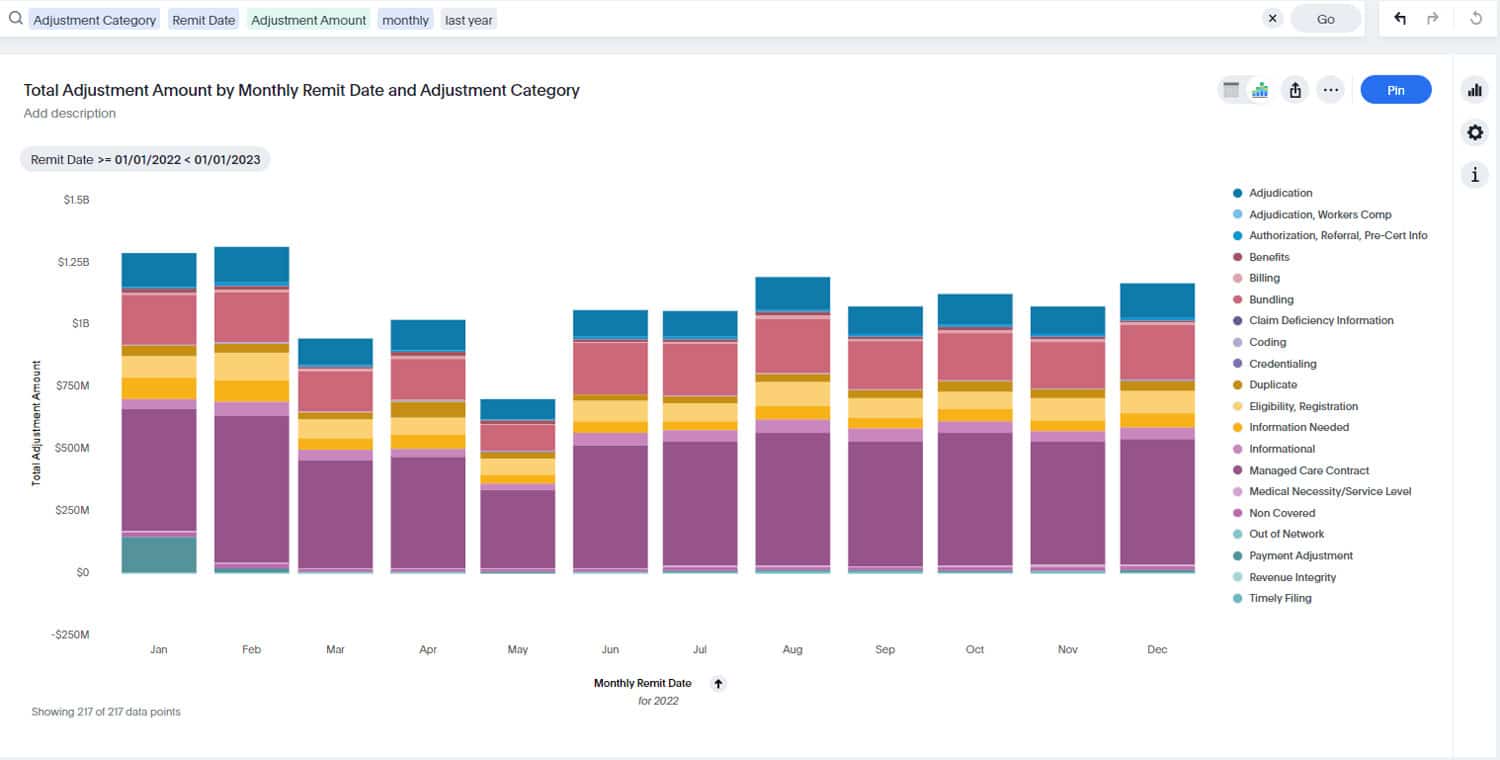
How MDaudit Turns Disparate Payer Rules Into One Analytics Fabric
MDaudit automates the ingestion of billing, coding, audit, and denial data from across the organization and applies analytics that illuminate patterns by payer, plan, service line, facility, provider, and coder.
Denials Predictor
Denials Predictor surfaces pre-payment risk at the charge level and explains the “why,” clarifying whether drivers are payer-specific (policy language, site-of-care restrictions, prior authorization) or systemic (documentation gaps, diagnosis specificity). Because it acts before adjudication, teams prevent avoidable denials instead of litigating them later.
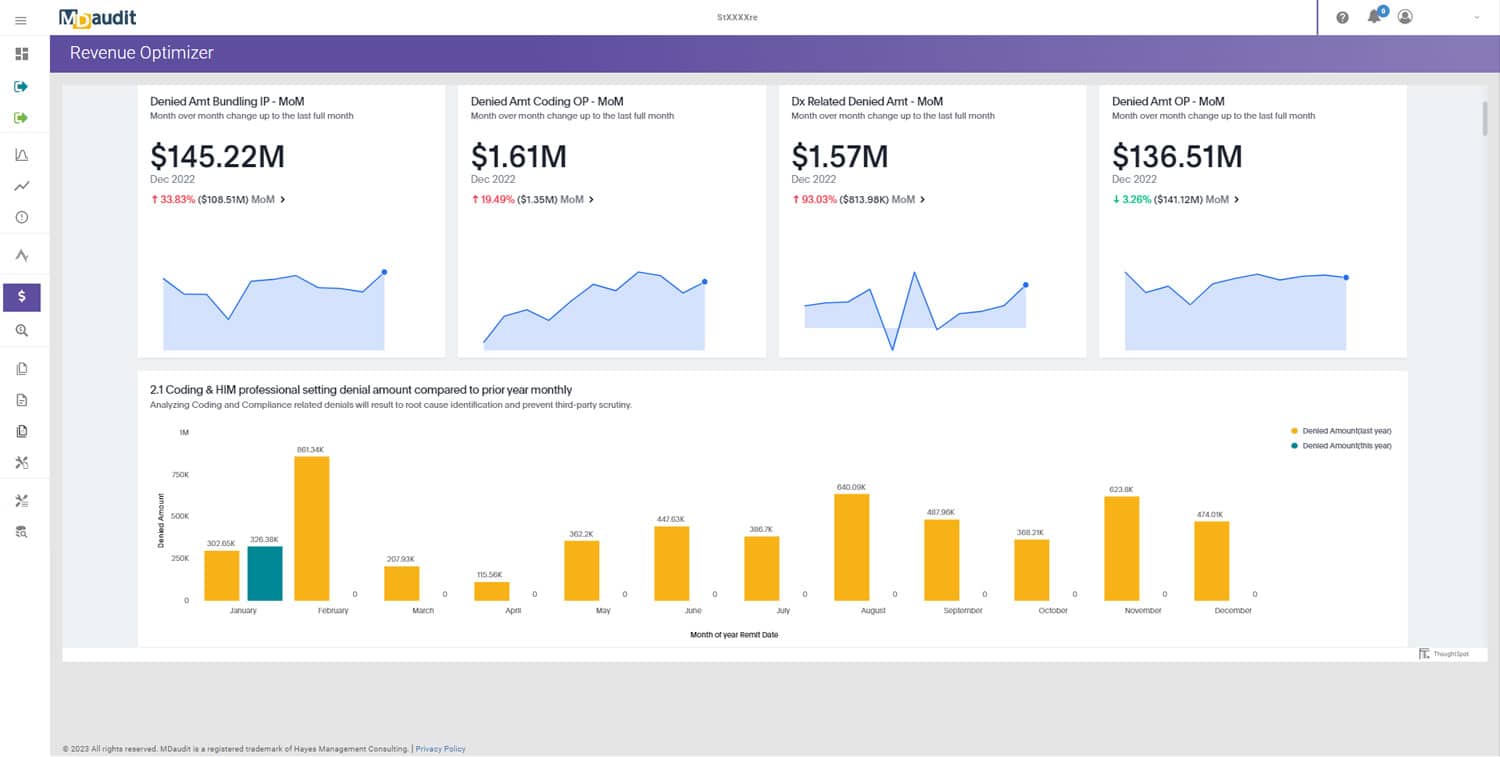
Revenue Optimizer
Revenue Optimizer quantifies impact by payer and service line, showing which denials cost the most, which interventions are paying off, and where to focus next. Results tie back to cash acceleration, overturn rates, and days in A/R.
Audit Workflows
Audit Workflows operationalize findings so issues route to the right owners with SLAs aligned to payer timelines, making follow-up timely and consistent.
Coder Workflow and HIM & Coding
For HIM and coding teams, cross-payer insights flow directly into Coder Workflow and the broader HIM & Coding toolkit, so education is targeted, rebuttals are structured, and feedback is immediate rather than months later.
Payer Audit Management
External requests and letters can be managed in the same framework with Payer Audit Management, so early signals from one carrier feed prevention across carriers.
Patterns That Only Appear When You Look Across Carriers
Medicare Versus Commercial Nuance
Medicare contractors may question cardiac procedures on NCD/LCD documentation elements, while a commercial payer focuses on prior authorization or frequency limits. Viewed separately, each denial feels different; looked at together, the pattern points to two complementary work streams: tighten documentation templates for Medicare populations and introduce scheduling hard stops for commercial plans that require pre-authorization.
Pharmacy and High-Cost Drugs
Specialty medications and infusion therapies drive a disproportionate share of denials. Multiple carriers often converge on the same themes—diagnosis specificity, step therapy, and site-of-care preference. Cross-payer analytics show when a concise documentation checklist or order-set update addresses most of the problem across all payers at once. For workflow context, see Navigating Complex Denial Management Workflows.
Inpatient DRG Downgrades
When several payers consistently question the same principal diagnoses with specific CC/MCC patterns, the signal is not just payer behavior; it is a documentation opportunity. Focused concurrent review and provider education reduce the issue across the board. Practical tactics appear in Effectively Managing DRG Downgrades with Technology.
Site-of-Care Shifts for Outpatient Infusions
Commercial payers continue to steer certain infusions away from hospital outpatient departments. Cross-payer trend lines show which drugs and diagnoses are targeted and how quickly policies shift. With that visibility, leaders can model revenue impact, revise scheduling guidelines, and equip access teams with payer-specific scripts.
Prior Authorization and Policy Drift
One payer tightens a rule in Q1; by Q2, two more follow. Cross-payer time series expose that drift early. The fix can be standardized—for example, adding required clinical evidence to the order—while routing exceptions through Audit Workflows for rapid review.
From Analytics to Action in Daily Operations
Analytics matter when they change the work people do today—not just what is reported next month. MDaudit ties cross-payer insights to the daily motion of compliance, HIM/coding, and revenue integrity.
Compliance and Internal Audit
Use cross-payer signals to prioritize samples by payer and service line, balance prospective and retrospective reviews, and shorten time from finding to fix. Execution guidance appears in Top 5 Ways Audit Workflow Automation Improves Compliance Efficiency, and the workflows that operationalize it are in Audit Workflows.
HIM and Coding
Route payer-specific trends into coder reviews and targeted education through Coder Workflow. When denial analytics show the same diagnosis pitfalls across three carriers, create a single education package, attach case examples, and measure post-education accuracy in subsequent audits. For broader context, see Coding/HIM Teams: Key Contributions and Challenges in the Revenue Cycle.
Revenue Integrity and Denials Prevention
Translate cross-payer patterns into pre-bill interventions. If prior authorization or medical necessity is the driver, embed checks upstream and use Denials Predictor to gate high-risk encounters before submission. Track downstream impact in Revenue Optimizer by payer, facility, and service line.
Executive Reporting and Contracting
Use cross-payer dashboards to quantify how denial rates, overturns, and days in A/R differ by carrier. The same evidence supports payer conversations, contract renegotiations, and carve-outs for site-of-care or prior-authorization requirements. For presentation techniques, see The Value of Data Visualizations and Reporting and Leveraging Revenue Integrity Reports for C-Suite Decision Making.
An Implementation Roadmap That Sticks
Start With a Focused Baseline
Use the reports described in 6 Claim Denial Reports for Revenue Integrity Teams to establish payer-level baselines: denial reasons, volumes, overturn rates, and average days in A/R for your top service lines. Resist the urge to boil the ocean. Choose two or three high-impact denial categories and your top four payers by volume or dollars at risk.
Wire the Insights Into Workflow
Create routing rules in Audit Workflows that assign payer-specific issues to the right owners with the right SLAs. If a commercial plan has a 14-day appeal window, build that timer into your rules so those items surface automatically. Attach education packages to each pattern so the fix becomes repeatable.
Layer In Pre-Payment Prediction
Once the foundation is stable, extend into prevention. Configure Denials Predictor for the targeted categories so you see high-risk encounters before adjudication.
Quantify and Communicate Results
Use Revenue Optimizer to attribute improvement to specific actions. Show reductions in predicted high-impact denials, improved first-pass yield, lower appeal volume, and net cash protected by payer. For broader framing, see Defining Revenue Integrity.
Expand Thoughtfully
Add adjacent service lines, bring in additional facilities, and tune thresholds as policies change. Formalize handoffs and escalation paths using the guidance in Understanding Claim Denials and Effective Routing Strategies, then revisit the rules set each quarter.
Governance That Prevents Backsliding
Ownership
Designate a small working group—revenue integrity, HIM, and compliance—with authority to set thresholds, approve education packages, and adjust routing. Publish a single change-control process so updates move quickly and transparently.
Cadence
Run monthly reviews focused on variance to targets by payer and denial category. Quarterly, re-baseline thresholds, refresh education content, and retire rules that no longer add value. Use Revenue Optimizer to keep the agenda outcome-oriented.
Escalation and SLA Design
Build auto-escalation for aging work and for high-dollar, time-sensitive categories. Where appeal windows are short, set tighter SLAs and create backup assignees by facility to prevent gaps.
Education Accountability
Tie each education package to a metric: post-education accuracy for the targeted cohort, reduction in repeat denials by payer and reason, or improvement in first-pass yield for the impacted services. If improvement stalls, revisit the content, delivery method, or upstream templates.
Case Snapshots
Integrated Delivery Network
Cross-payer analytics showed infusion denials tied to diagnosis specificity rising with three commercial plans while Medicare remained stable. Access added a hard-stop at scheduling, HIM refreshed coder guidance, and pharmacy updated order sets. Within one quarter, high-impact denials fell across all three plans, and the appeal workload dropped.
Academic Medical Center
DRG downgrades clustered around a narrow set of MCC codes across Medicare Advantage and two commercial carriers. Concurrent review focused on those combinations, providers received short in-service sessions, and CDI added admission-order checklists. Downgrades declined and documentation-related revenue leakage eased, consistent with the tactics in Effectively Managing DRG Downgrades with Technology.
Large Physician Group
A cross-payer view highlighted one carrier denying advanced imaging at triple the rate of others. Evidence supported a contract discussion and a documentation refresh for all carriers. Denial rates normalized, and the renegotiated terms improved predictability in cash.
Where AI Accelerates Cross-Payer Strategy—Without Losing Human Judgment
We design AI to compress time to insight while keeping experts in control. Our approach in AI-Powered Technology clusters similar denials across carriers, highlights emerging patterns, and drafts suggested playbooks. Auditors, HIM leaders, and revenue integrity managers review the rationale, refine the plan, and approve the workflow.
Data Foundations That Make Cross-Payer Analytics Reliable
Raw denial codes and reason texts vary by payer. To compare apples to apples, normalize reason codes into a unified taxonomy and enrich each denial with context: expected dollar impact, likelihood to overturn, and appeal window. That standardization is what turns a pile of rejections into a strategic dataset. Within MDaudit, normalization and enrichment flow into working queues, so staff see not only what happened but what to do next and by when.
Ten-Day Sprint to Visible Value
Day 1–2: stand up payer-level baselines in Revenue Optimizer for two high-impact categories.
Day 3–4: write routing rules in Audit Workflows and attach education modules from Coder Workflow.
Day 5–6: configure Denials Predictor for those categories; pilot at one facility.
Day 7–8: hold short huddles with compliance, HIM, and revenue integrity; review the first wave of signals, close gaps, and confirm SLAs.
Day 9–10: publish a one-page summary on expected dollar impact and set the cadence for the next review.
Getting Started
To see cross-payer analytics tied directly to daily work, request a session on our demo request page or reach out through contact us. We will align on goals, configure a focused baseline, and show how the combination of Denials Predictor, Revenue Optimizer, Audit Workflows, Payer Audit Management, and Coder Workflow turns payer variability into a single, repeatable strategy.