Executive Blog Summary
Healthcare CFOs are navigating tighter margins, increasing regulatory scrutiny, and rising complexity across revenue cycle operations. Before investing in any compliance or revenue integrity technology, they want to know: Will this platform make a measurable difference?
MDaudit was purpose-built to answer that question. Below, we address the seven most pressing concerns CFOs have when evaluating a strategic solution like MDaudit.
Questions:
How will MDaudit directly impact our bottom line?
What proof do you have that MDaudit improves compliance and mitigates audit risk?
How does MDaudit integrate with our existing systems and workflows?
What kind of visibility will I have into financial risk and performance trends?
What do similar organizations gain from using MDaudit?
What’s the future of MDaudit when it comes to AI?
Is MDaudit an end-to-end solution?
1. How will MDaudit directly impact our bottom line?
CFOs want technology that delivers results—specifically, better margins and less revenue loss.
MDaudit continuously monitors your financial data, including claims and payments, to uncover coding and billing errors across the enterprise. It also identifies improper payments, both over and under. By surfacing these insights and enabling both near-term fixes and long-term process improvements, MDaudit directly contributes to stronger financial performance.
2. What proof do you have that MDaudit improves compliance and mitigates audit risk?
MDaudit is trusted by some of the largest and most complex healthcare organizations in the country, and the numbers speak for themselves.
MDaudit by the numbers (past 12 months):
- Used by 70+ leading health systems with over $1B in Net Patient Revenue
- Supports 800K+ physicians, 4,000+ facilities, and 1,500+ auditors
- $13B in charges audited through the platform
- $2.8B flagged for underpayments, overpayments, and EMR edit issues
- $262M in revenue retained from payer audits using the Payer Audit Workflow solution
3. How does MDaudit integrate with our existing systems and workflows?
Interoperability and ease of implementation are crucial for healthcare CFOs evaluating new technology.
MDaudit is designed to work seamlessly across diverse health IT environments. Our customers typically manage 6-8 EMRs, including Epic, Cerner, Meditech, and eClinicalWorks. The platform consolidates disparate billing and coding data into a unified view, giving compliance and revenue integrity teams enterprise-wide visibility.
Additionally, MDaudit offers outbound APIs for data integration into operational systems, further streamlining your tech stack.
4. What kind of visibility will I have into financial risk and performance trends?
CFOs need more than static reports; they need real-time, actionable intelligence.
MDaudit delivers best-in-class reporting and analytics through management dashboards, Adhoc reports, and interactive visualizations. These are tightly integrated into the platform’s automation workflows, enabling teams to move from insight to action quickly.
Example modules delivering executive-level visibility:
- Billing Risks – Identifies anomalies with your charge data across professional and hospital settings and services
- Revenue Optimizer – Identifies root cause of denials across your enterprise across 30+ dimensions in real-time
- Denials Predictor – Flags claims that can be fixed for medical necessity and information needed issues before being routed for payment
Use Case Examples:
- Within the first three quarters following implementation, this Southeastern Mid-Sized Hospital audited $2.7M in charges, with 38% resulting in unsatisfactory outcomes. Of the 1.4K unsatisfactory findings, 40% identified undercoded E&M as the reason, and 37% cited overcoded E&M.
- A Non-Profit Health System experiences a $9M decrease in denials associated with PB Coding, thanks to MDaudit’s Revenue Optimizer.
- Faith-Based, Nonprofit uses MDaudit’s Revenue Integrity Suite and Denials Predictor to identify nearly 23% more revenue while decreasing compliance risk by 20%.
5. What do similar organizations gain from using MDaudit?
For CFOs, benchmarking performance is just as important as improving it. The MDaudit Community has a nationwide footprint, with over 170+ healthcare organizations across the U.S. This includes 70 of the top 100 IDNs (Integrated Delivery Networks) in the country.
Within this community, there is a wealth of data that can be used for benchmarking to understand how your respective organization is performing compared to other organizations like yours. Real-time access to this data allows organizations to identify risks, maximize revenues, and gain strategic insights on how to recognize healthier bottom lines.
MDaudit’s annual benchmarking report is a goldmine of peer data, performance metrics, and trends across billing compliance, coding accuracy, and revenue integrity. The insights in this report show how leading healthcare organizations are protecting millions in revenue while scaling compliance operations efficiently.
Sample Insights (2024 Benchmark Report):
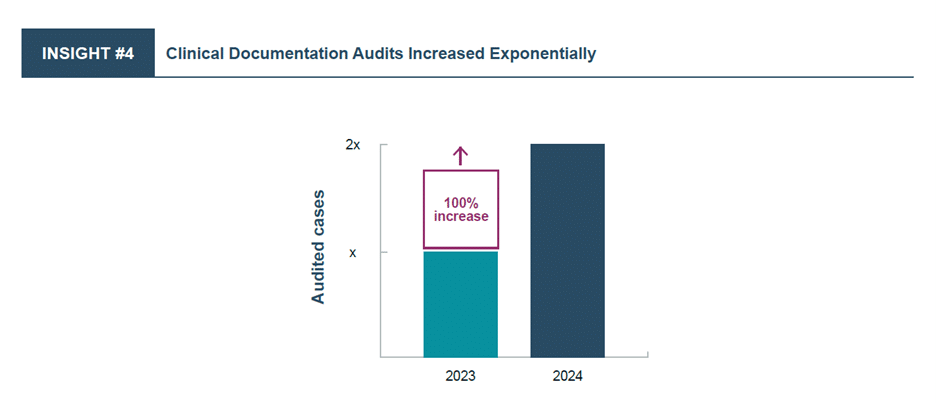
Billing Compliance Insight: Clinical documentation audits and reviews surged by 100% in 2024 vs. 2023. According to MDaudit data, clinical denials have increased 51% in the last three years.
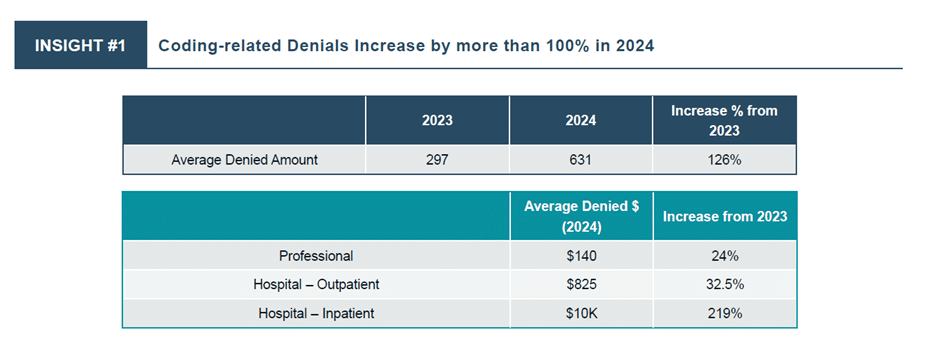
HIM/Coding Insight: Coding remains one of the biggest improvement opportunities for revenue capture and margin expansion. Despite billions of dollars spent on outsourcing coding operations and investing in automated coding technologies, the average denied amount increased by 126% in 2024 vs. 2023.
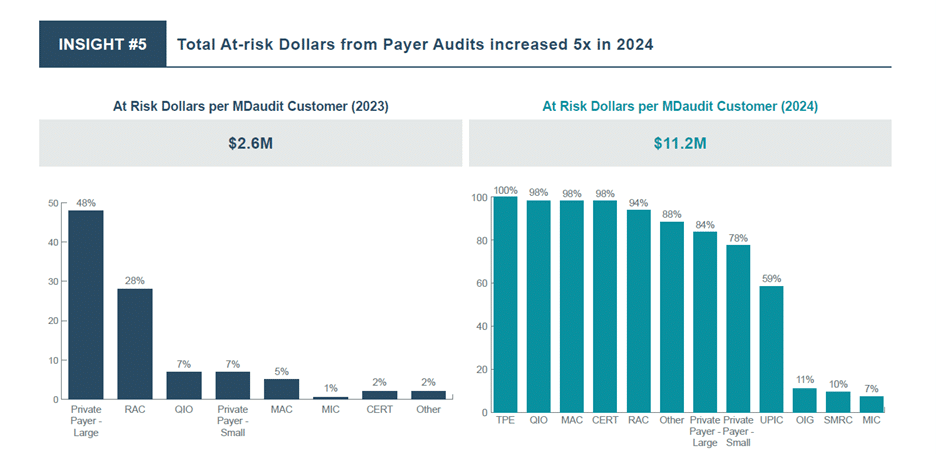
Revenue Integrity Insight: External Payer Audits increased nearly 5x in terms of at-risk dollars in 2024 vs. 2023. The average at-risk dollar per customer in the MDaudit community increased from $2.M to almost $11.2M.
You can find the latest report available for download here.
6. What’s the future of MDaudit when it comes to AI?
MDaudit is leading the way in applying Meaningful AI to revenue cycle management, with a focus on business outcomes and “humans in the loop.”
Defining Meaningful AI at MDaudit
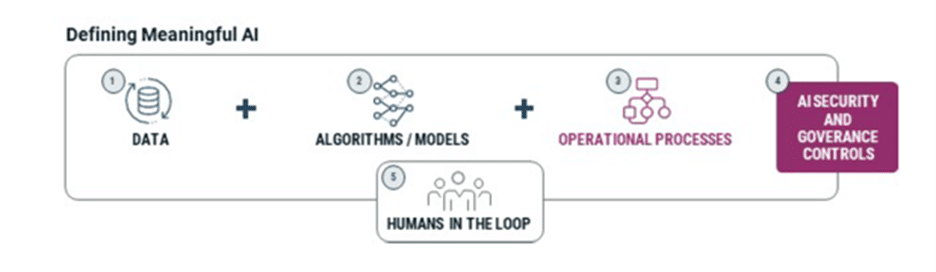
Our AI strategy centers on three goals:
- Enable revenue capture
- Mitigate financial risk
- Improve operational efficiency
AI-driven innovations in action:
AI-Assist – MDaudit’s AI Assist works with your team to transform overwhelming claims, denial remittances, audits, and financial data into simple, smart, actionable insights in seconds, not days or weeks. Users can ask complex questions —no AI expertise required—and receive instant, simple, data-driven answers. Whether identifying top denial drivers, tracking audit outcomes, or uncovering revenue opportunities, AI Assist empowers your team to mitigate risk, optimize revenue, and make smarter decisions faster than ever.
SmartScan.ai – Within the Payer Audit Management module, this intelligent functionality allows users to upload payer request letters, which are parsed to extract relevant attributes for case searches, enabling a much simpler search. This eliminates tedious manual work, adding an iterative case search process with more flexibility and expediting the overall resolution of audits.
These AI tools help organizations stay ahead of payer trends, reduce audit response times, and improve team productivity.
7. Is MDaudit an end-to-end solution?
Yes, MDaudit is an enterprise-grade platform that spans the mid and back of the revenue cycle. We offer 10 distinct workflow and analytics modules that support billing compliance, HIM/coding, and revenue integrity teams. With more than 4,000+ active users, MDaudit connects audit management, risk identification, payer audit tracking, denial prevention, and reporting in one place.
Final Thoughts
Your CFO is right to ask tough questions. MDaudit is built to answer them with measurable value, enterprise-grade analytics, and a forward-looking approach to AI.
Whether you’re facing mounting payer audits, increasing coding complexity, or compliance resource strain, MDaudit helps you protect revenue, minimize risk, and operate more efficiently.
Want to learn more? Contact us to see how MDaudit fits your revenue cycle needs and financial strategy.