THE CUSTOMER PROFILE
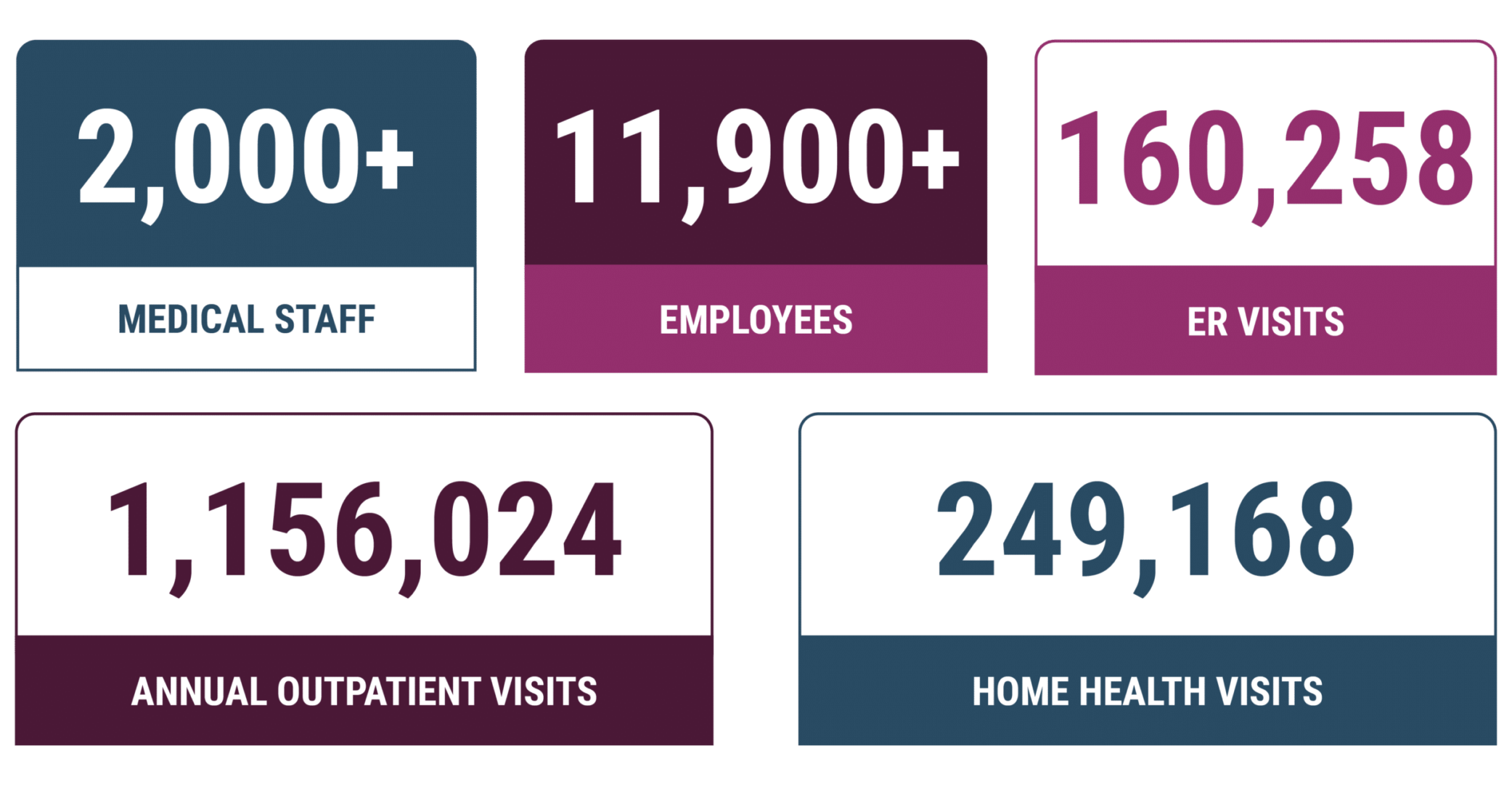
With five hospitals, six health centers, and 40+ offices, Main Line Health is a not-for-profit health system that has provided safe, highquality health services to Philadelphia and its suburbs since 1985. Four of Main Line’s five hospitals rank among the top acute care hospitals in the Philadelphia region by U.S. News and World Report. The fifth, Bryn Mawr Rehabilitation Hospital, is one of the nation’s premier facilities for rehabilitative medicine.
In addition, Main Line has received national recognition for nursing excellence, patient safety and transparency, equity and inclusion, and cardiovascular care, among other honors. Many of its 2,000+ physicians are ranked among the Top Doctors by Philadelphia and Main Line Today magazines.
THE CHALLENGE
Amid economic challenges, Main Line Health needed tools for minimizing compliance risk and systematizing provider education.
“Every health system today is struggling. We’re struggling. Everybody’s struggling. We have to find whatever we can find. Anywhere we can find it,” says Karen Gallagher, compliance audit manager at Main Line Health.
In an increasingly precarious post-COVID healthcare environment where every dollar counts, healthcare organizations must protect the bottom line by going beyond minimizing compliance risk associated with overcoding. Today, billing compliance departments are being called on to break down silos and identify opportunities for their organizations to maximize revenues in new and creative ways.
Like many other health systems, Main Line Health had to focus its limited compliance resources on scheduled audits, sacrificing the benefits of a broader risk-based strategy incorporating both prospective and retrospective audits to eradicate issues before they can negatively impact revenues. “We were only able to run a basic audit routine,” explains Gallagher.
Access to real-time analytics is a crucial first step in enabling healthcare billing compliance, revenue cycle, and revenue integrity managers and executives to monitor billing risk, detect anomalies, provide insights, and implement corrective action.
New providers are known to present specific compliance risks – even for reasons as simple as learning the nuances of the facility’s electronic health record system. Previously, there was no clear notification to the compliance department when new providers joined Main Line. As a result, it could take up to four months to incorporate them into the auditing program. Within that timeframe, HMOs expire, claim deadlines pass, and a host of other problems are created. “I’ve seen new providers get health systems into trouble before,” says Gallagher.
Every July, residents become new doctors, and there is a new class of residents. This significant change in Main Line’s provider population makes prospective audits of new providers even more important to the non-profit training hospital.
THE SOLUTION
MDaudit increased audits and made them and provider
engagement more meaningful for long-term impact.
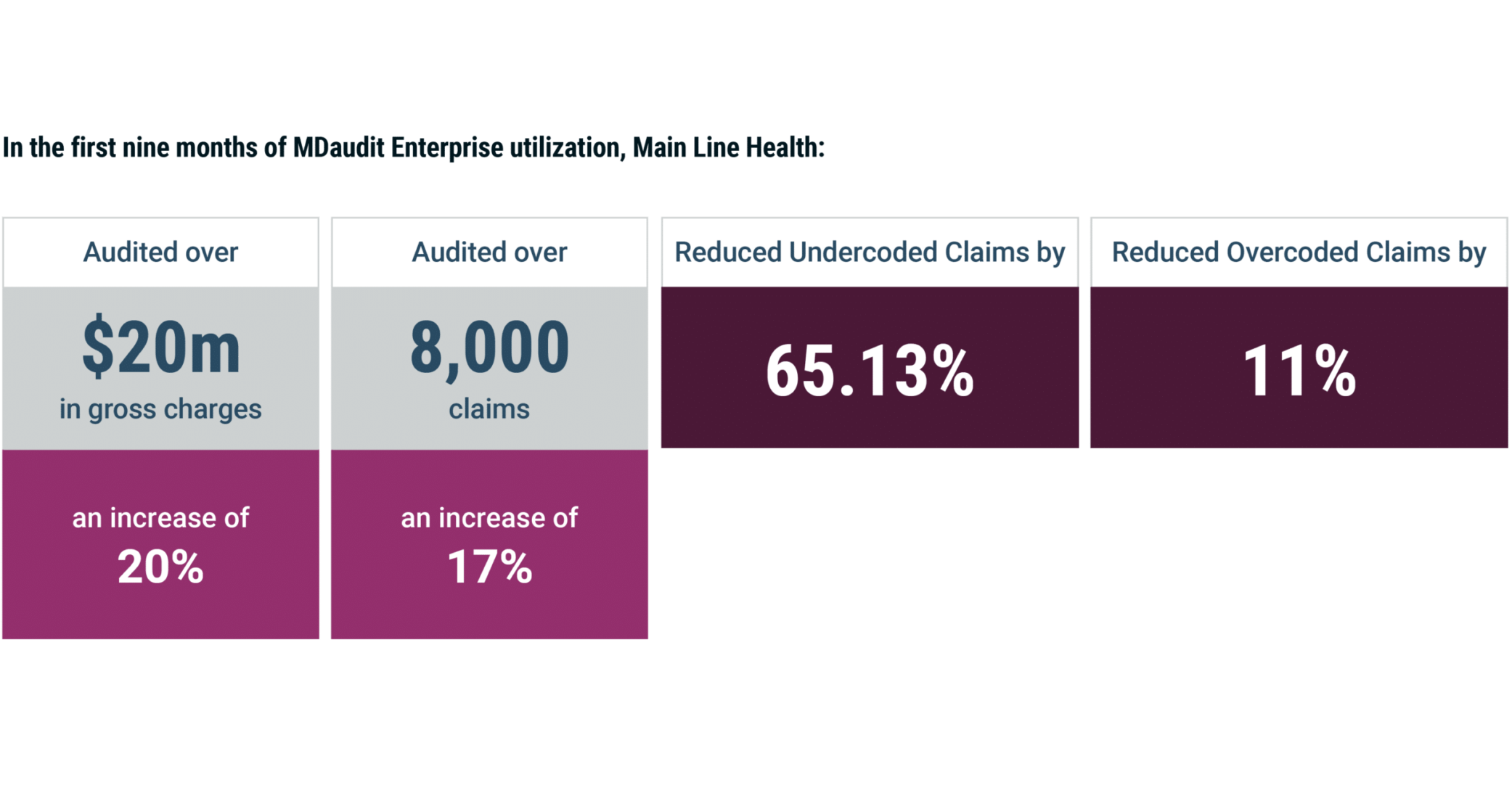
In the nine months since utilizing MDaudit in May of 2022, Main Line audited over 8,000 claims, representing a 17% increase in total claims audited and pushing total charges audited up by 20% to $20 million.
Main Line leverages Risk Stratification in the Billing Risks Module of MDaudit to identify their top 10 high billers and top 10 undercoders. It has also accelerated integration of new providers into the auditing program, allowing the compliance department to “get them in and through the system and coding more in accordance with the acuity and complexity of the care that they’re providing, rather than just being a middle lane driver,”
says Gallagher.
With MDaudit, one new provider appeared in the Billing Risk list within her first week when she attempted to enter 42 post-op visits into Main Line’s Epic system, but mistakenly did so in a way that would have resulted in
no charges being billed.
“Because it was in MDaudit, I was able to catch and correct it and get her the Epic training she needed,” says Gallagher. “Those 42 visits could have represented $50,000 lost had they not been caught, and it could have easily gone into the millions. Because they were zero-charge claims, they never would have been found.”
She adds, “When we talk about MDaudit, we talk about it in terms of the data in the system, but the other side of that coin is how it enables us to identify systemic problems. We’ve been able to decrease our undercoding
by 65%, not counting provider patterns going forward. Even more important than rebilling one insurance company $500 for a provider, we can see that provider generate $5,000 more in valuable income by coding appropriately moving forward. The undercoding is important, but the real value that I see is in the long term.”
Perhaps more impressive than the purely numerical aspect, however, is MDaudit’s impact on provider education. When particular procedures become subject to external audits, identifying and engaging with the providers performing those procedures falls to compliance.
MDaudit’s multiple objective risk assessment tools allow auditors to work with practice staff and develop mitigation plans, preventing adverse audit findings and providing better provider education.
“The biggest value that I’ve seen is the physician engagement,” says Gallagher. “I’m not a punitive person. I don’t like that. When you can address a provider with respect and data, you have that relationship with them for life.”
Better relationships with providers mean more effective root-cause analysis and correction, preventing coding errors at the source and resulting in incalculable reductions in lost revenue and compliance risk. Providing insights into audit outcomes and accuracy rates for provider, coder, and facility audits also drastically improves Main Line’s compliance department’s capacity to prioritize the millions of line items that go into every internal audit.
Additional revenue opportunities also become available when the scale and efficacy of audits are increased. For example, Main Line Health has increased its specialty and subspecialty services over the years. With changes in telehealth, opioid use disorder, and other similar programs with complex regulations that vary from state to state, managing claims for specialties like behavioral health presents a wide array of new and varied compliance concerns. “Without MDaudit, we wouldn’t be able to manage it,” explains Gallagher. “There isn’t another compliance platform that matches MDaudit on provider billing.”
While revenues and control over auditor workflows are important, Gallagher says the greatest value MDaudit delivers is physician engagement. It allows the compliance team to work one-on-one with providers, to understand their concerns and educate them on compliant approaches to resolving them.
“It used to be that we would just focus on overcoding. We can’t do that anymore. We can’t. The economic situation of the industry does not allow it,” she says. “By building relationships with providers and our health system leadership, we can make a difference.”

THE RESULTS