THE CUSTOMER PROFILE
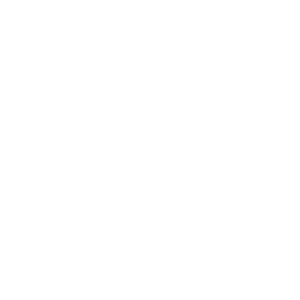
Serving 12 communities across the Midwest, this large health system offers more than 30 medical specialties. The organization comprises five hospitals and 40-plus medical clinics/specialty centers and employs over 5,000 physicians and caregivers.
The health system is a member of the Mayo Clinic Care Network and is committed to delivering high-quality care, providing a caring experience, being a great place to work, and positively impacting its communities. It has received many accolades for its cardiovascular care, as well as for stroke treatment and maternity care.
THE CHALLENGE
Deep personnel cuts result in a laser focus on identifying risk and leaning hard on technology to improve efficiencies.
Being asked to do more with less is a common theme in non-clinical healthcare departments these days. At this particular organization, that ask has been extreme, with compliance department personnel reductions and significant data responsibilities being added to the already small revenue cycle management team.
“We are down three team members, so we’re working on how to get the same amount of work done by increasing efficiency,” says its compliance specialist. In large part, that means identifying areas of high risk, including providers who are over- or undercoding, and detecting patterns of denials. She and her team are also working on systems to help catch claim errors before they are sent to the clearinghouse, reducing the need for rework.
The department’s internal audit specialist agrees. “We’re experiencing a great deal of change, but that’s a huge opportunity to improve processes we haven’t looked at before because we need to create those efficiencies,” he says. “I believe risk-based auditing is where we need to go.”
One focus area for him is denials reduction. He says every avoided denial saves the organization between $100 and $1,000, depending on how much time it would take to fix the claim. He’s also interested in demonstrating that while the compliance department technically doesn’t produce revenue, it has a substantial impact on the medical system’s bottom line.
As far as the compliance department goes, one of our battles is the fact that we are not a revenue-producing department. But I think we could argue that, in some ways, we really are.
Instead of having to re-audit three or six months after providing education to a clinician or coder, we can use analytics to see if their numbers are trending in the right direction. That takes minutes instead of hours or days.
THE SOLUTION
MDaudit has increased efficiency by lowering denial rates, identifying more risk, reducing re-audits, and simplifying report creation.
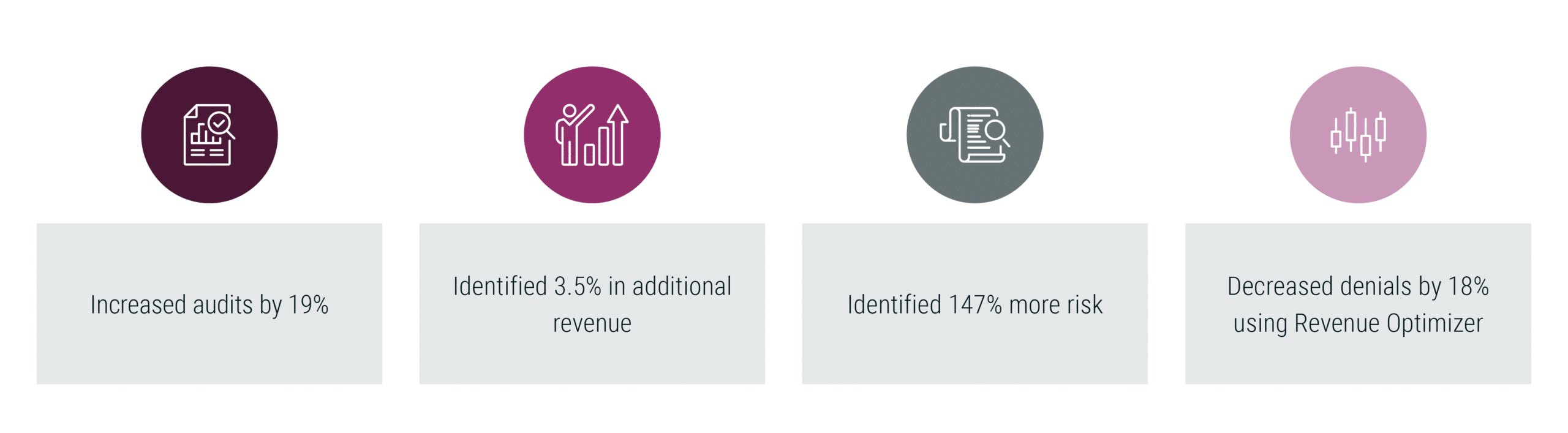
The organization has been using MDaudit since 2011 and upgraded to the enterprise version in 2020. That turned out to be a prophetic move, as both compliance specialists and internal auditors can employ its workflows and analytics to greatly improve efficiency in the face of layoffs. The number of audits conducted by the department increased by 19% from 2021 to 2022, identifying 3.5% in additional revenue and 147% more risk.
MDaudit gave both the internal audit specialist and the compliance specialist a much clearer picture of which providers are most at risk of undercoding. “MDaudit allows us to identify those compliance risks and mitigate them. It has definitely helped us shift to prospective rather than retrospective audits.”
Just as important, data analytics keeps everything moving in the right direction. “Instead of having to re-audit three or six months after providing education to a clinician or coder, we can use analytics to see if their numbers are trending in the right direction,” says the compliance specialist. “That takes minutes instead of hours or days.”
The health system has also seen an 18% drop in denials, which the audit specialist attributes to MDaudit’s Revenue Optimizer module. “For example, I’ve been looking at timely filing, and MDaudit was a big help,” he says. “I was able to easily identify which reason codes and remark codes to start with and quickly drill down into dollar amounts and volume.”
MDaudit’s reporting features are also a boon to the organization. For one thing, he can create charts showing weekly, monthly, or quarterly audit numbers to help compliance staff understand trends. For another, he can pull together all the data compliance personnel need for focused audits and easily create a PDF to show a provider group where it sits on the risk bell curve. Finally, he can use MDaudit’s analysis tools to better communicate with other departments.
“This tool brings everything all together in a way I’ve never seen before,” he says. “And it’s a huge timesaver to be able to provide a summary of the trends we’re seeing to the health information management, finance, and revenue integrity departments so we can all be on the same page.”
THE RESULTS
From 2021 to 22:
To download the full case study PDF, click here.