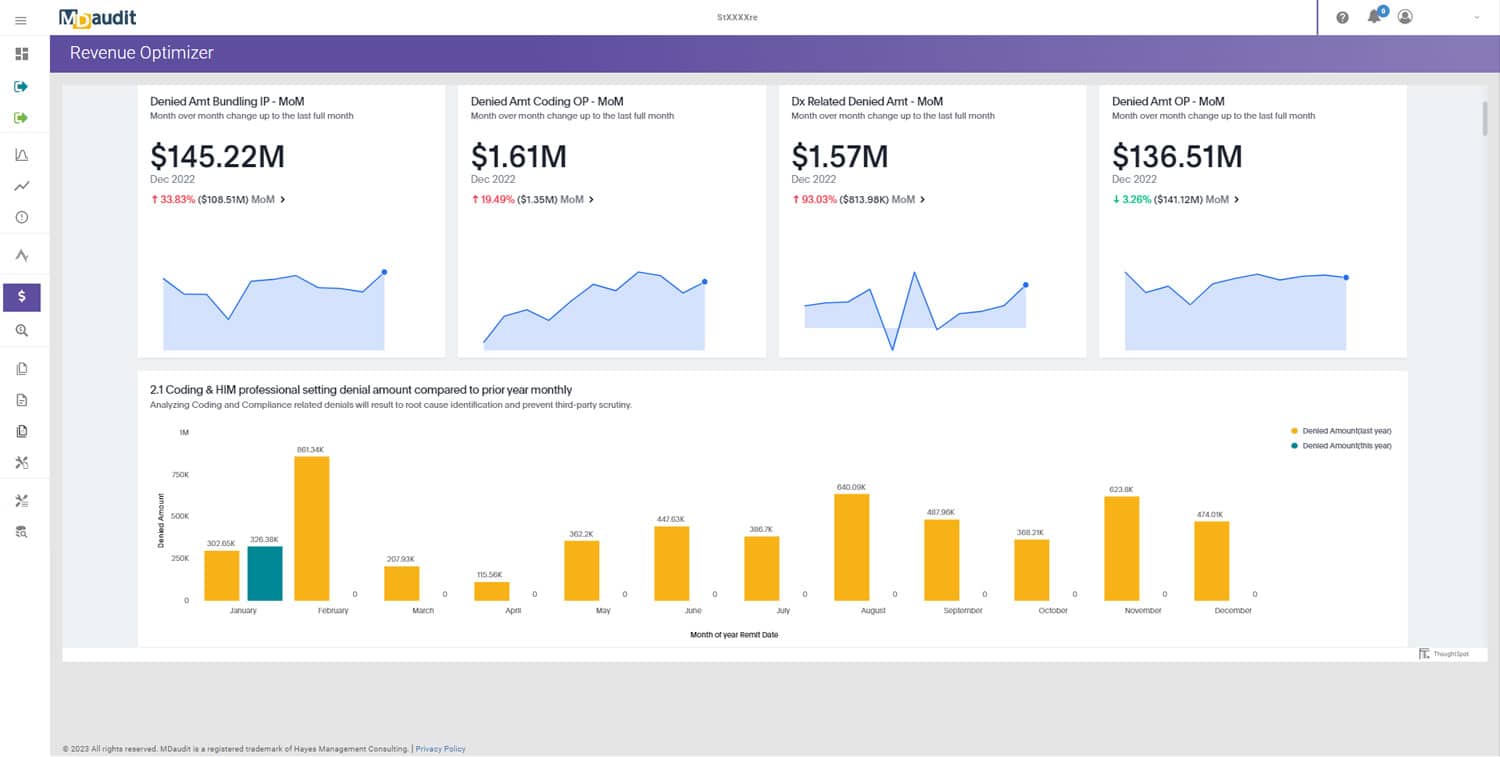
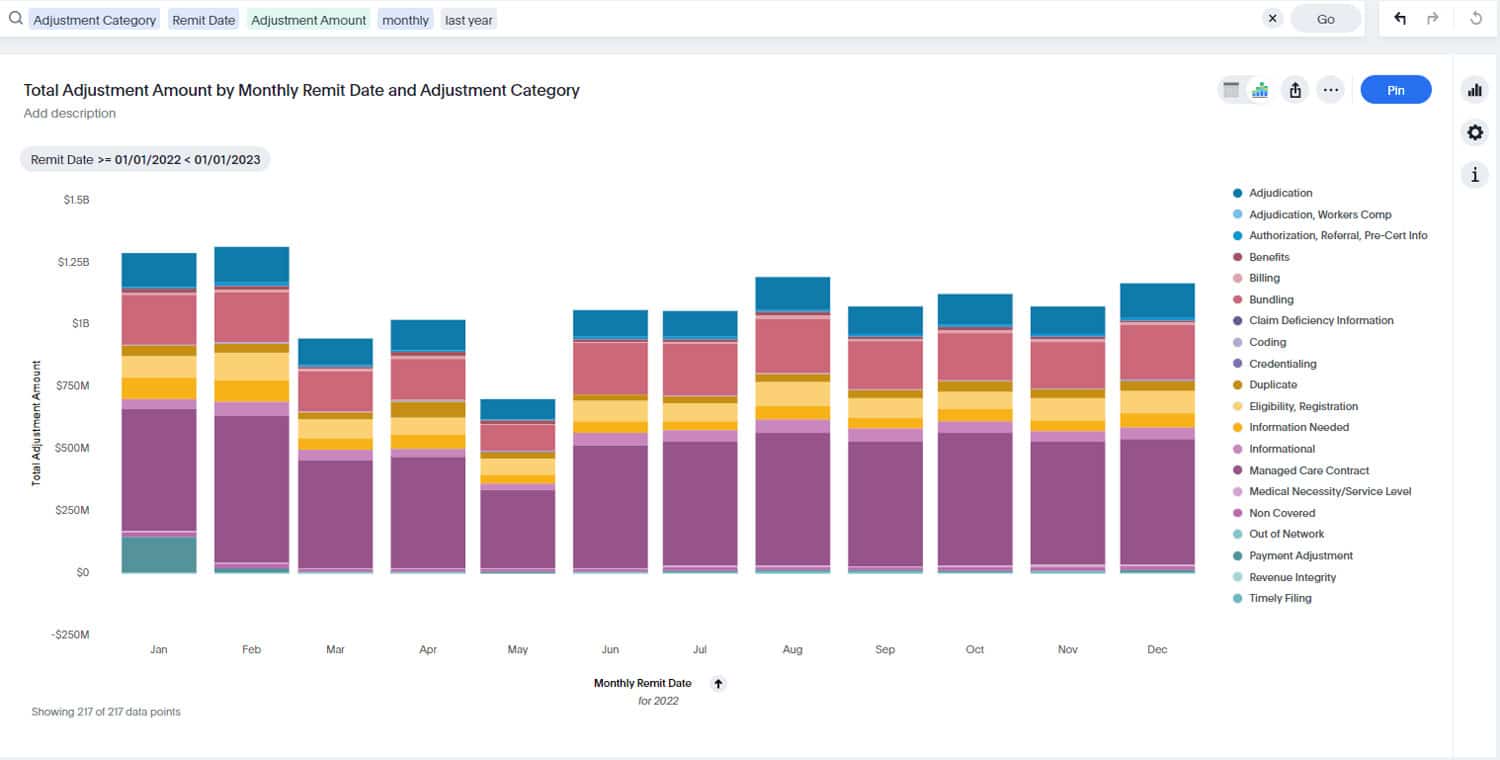
MDaudit is featured in Healthcare Business Today for its 2024 Annual Benchmark Report, which reveals a fivefold increase in dollars at risk from payer audits and a surge of over 125% in coding-related denials. The report indicates that external audit volumes more than doubled in 2024 compared to 2023, with total at-risk dollars reaching $11.2 million per MDaudit customer. These findings underscore the pressing need for healthcare organizations to overhaul their revenue cycle management (RCM) strategies to mitigate financial risks and improve cash flow stability.
The report also highlights a significant rise in medical necessity-related denials—75% for outpatient claims and 140% for inpatient claims—further emphasizing the challenges faced by healthcare providers. To address these issues, MDaudit recommends a hybrid auditing strategy that combines retrospective and prospective audits, leveraging technology and analytics to proactively identify and correct billing errors. CEO Ritesh Ramesh emphasizes that investing in real-time monitoring of billing risks and integrating clinical documentation improvement (CDI), billing, coding, and RCM programs are crucial steps toward achieving financial resilience in 2025.
Read the full article here: MDaudit’s 2024 Benchmark Report Reveals a Fivefold Increase in Dollars At-Risk from Payer Audits While Coding-Related Denials Surged by Over 125%.