This is part three in a three-part series examining denials prevention, including the use of technology, payers’ ever-changing rules, and managing workflows for maximum efficiency.
Denial rates continue to rise and payers are increasing investments in advanced technologies to further scrutinize claims in the future. In the first three quarters of 2022, a staggering 82% of initial claims were rejected by Medicare Part A and Part B payers. As the number of denials is growing, so too is the dollar amount – the average amount of hospital inpatient charges denied has increased by nearly 10% since last year, to more than $5800. More than ever, preserving health system revenue is as important as growing revenue.
Avoiding denials and increasing first-pass payments are the most effective way to protect revenue integrity. This requires the cleanest, most accurate claims possible, but with so many charges streaming through a health system on any given day, implementing effective and efficient revenue integrity workflows is crucial.
As revenue teams face ongoing resource constraints, identifying and prioritizing the greatest denials risk can allow health systems to focus strategically on the most impactful source of claims denials.
MAXIMIZE IMPACT
Knowing that as little as 20% of denials volume can drive as much as 80% of denials dollar amounts, smart health systems are finding ways to maximize limited staff resources by developing workflows that give special attention to those claims with the most significant impact on their bottom line.
Claim scrubbers are a good first step. But as we discussed in part one of this blog series, claim scrubbers still miss a lot of reasons for high-dollar denials. Payer-driven rules engines are a tremendous game-changer in avoiding denials, but even they require some level of human review and corrections.
With teams stretched thinner than ever, there are three key approaches to optimally identifying and prioritizing denials risk:
- Leverage data analytics to diagnose denials trends
- Prospectively audit claims to proactively mitigate denials
- Employ risk-based audits and subsequent education to address systemic issues
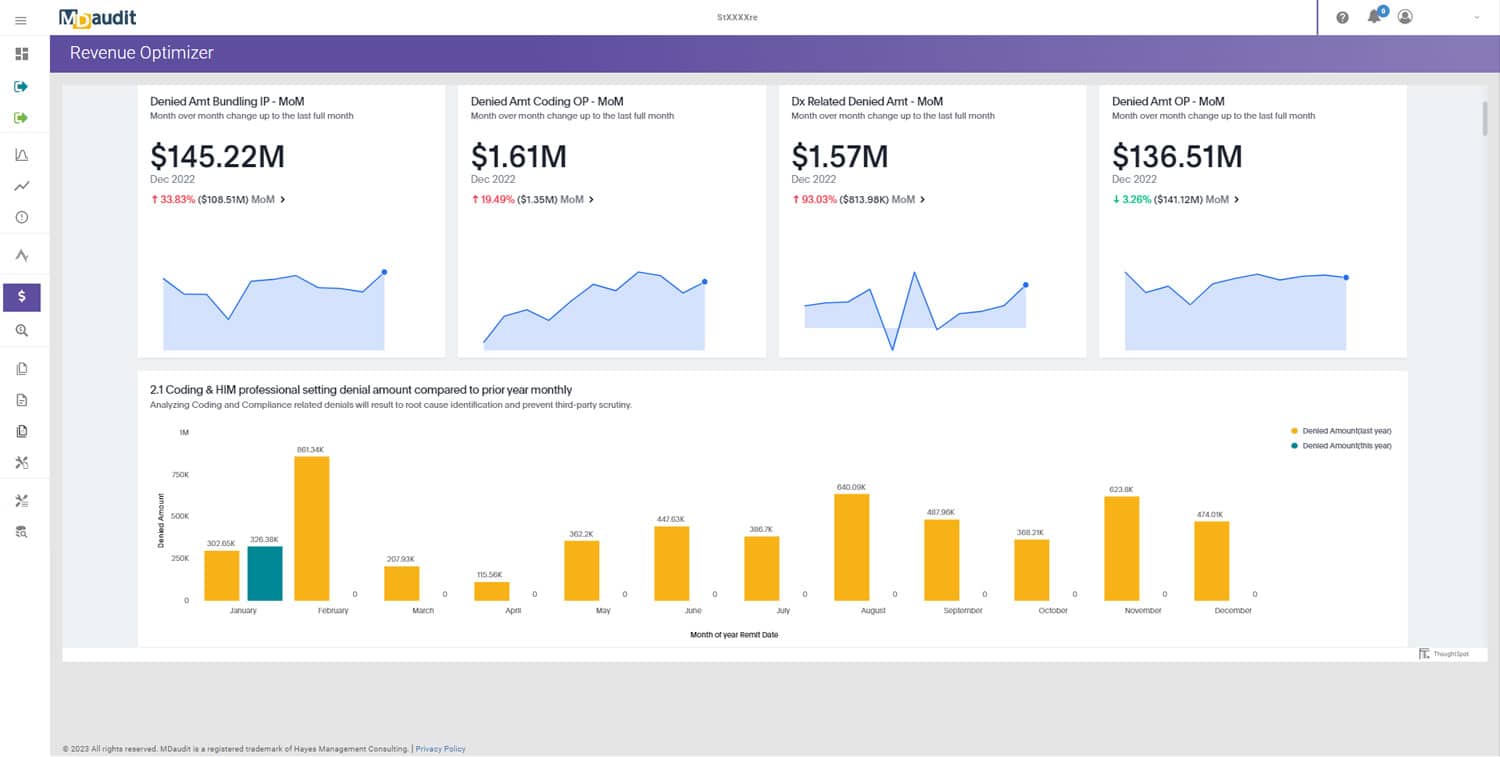
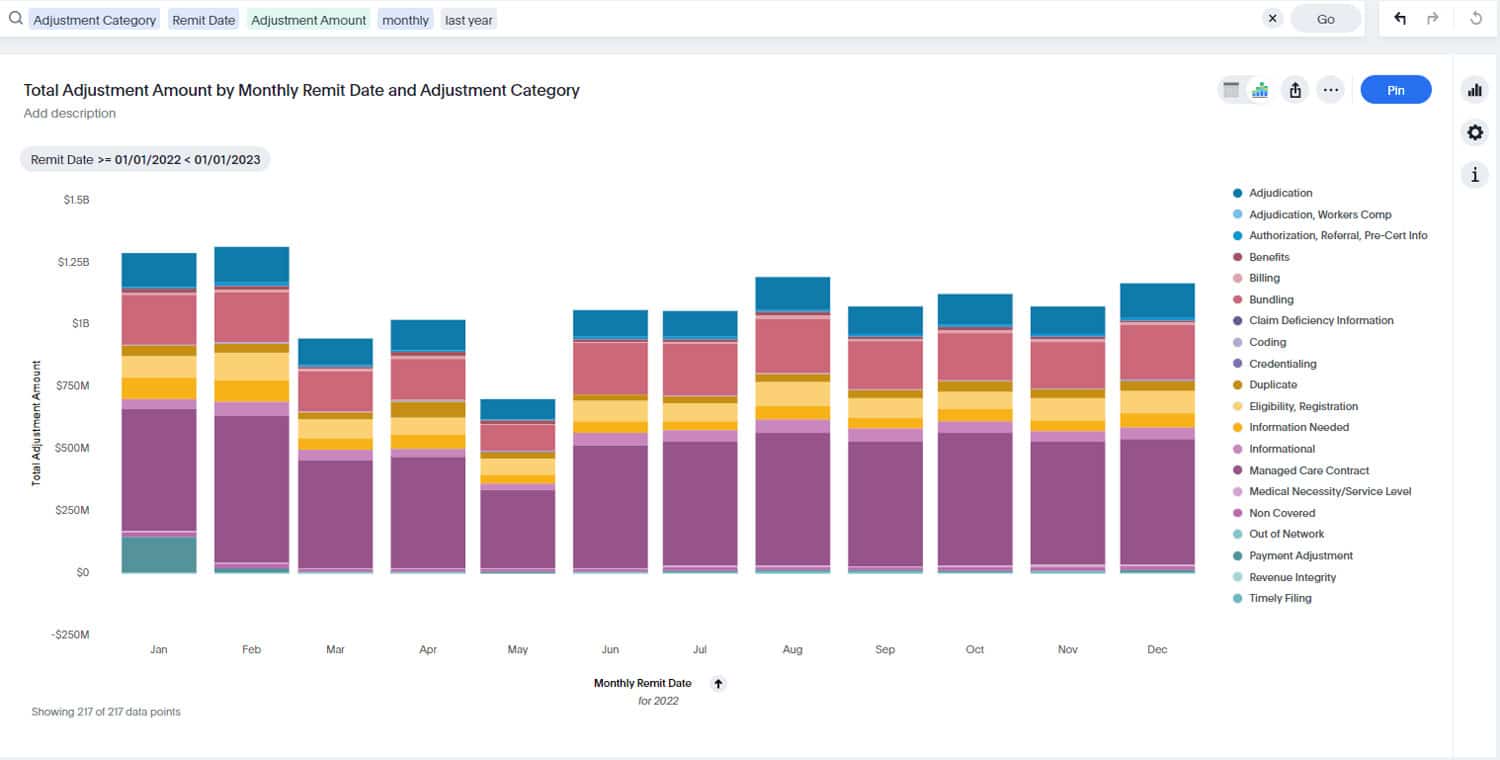
IDENTIFY & PRIORITIZE DENIALS TRENDS
Advanced data analytics can offer meaningful insights using remittance data to diagnose systemic denials trends and monitor the effectiveness of mitigation programs. By identifying and reporting on the most important denial trends affecting compliance and revenue, focus can be given to high-risk areas to correct issues before they occur – preventing revenue loss and reducing the time spent in accounts receivable to accelerate cash flow.
PROACTIVELY MITIGATE DENIALS
Prospective auditing offers auditors an opportunity to review charges before the bill is sent out to the payers and prevent problematic claims from being submitted and subsequently denied. Increasingly, teams are taking adding prospective audits to existing retrospective audit workflows to proactively mitigate compliance and revenue issues.
Prospective audits account for 31% of all professional, hospital, and coding audits performed this year – up more than 20% from last year.
FOCUS ON SYSTEMIC RISKS
Preventing billing errors before they occur is the most efficient means of mitigating denials. Risked-based audits address potential problem areas preemptively, stopping them from becoming more serious revenue and compliance issues. This workflow makes eases the burden of discovering and resolving issues, saving health systems time and money.
Due to the dynamic nature of emerging risks, revenue integrity teams must rely on real-time data and analytics at scale across their organizations to detect risks. When combined with proactive measures and ongoing monitoring, risk-based audits help to improve revenue flow by changing billing practices before errors are made.
Risk-based audits have increased by 28% across professional and hospital billing as compared to 2021.
GET IT RIGHT
Effective revenue integrity workflows require the right technology, subject matter expertise, and collaboration and communication between departments. Together, revenue integrity teams can identify, prioritize, and address systemic denial risks with the most significant financial impact, maximizing precious resources where they are needed most.MDaudit’s cloud-based Revenue Integrity Suite automates an end-to-end denials prevention process that uniquely leverages payer remits to diagnose systemic risk based on trends, applies those insights to pre-bill charges to identify potential denials, and recommends erroneous claims for proactive audit and corrections before releasing to payers, resulting in lower denials.
Schedule a demo to learn how the Revenue Integrity Suite puts analytics into action to prevent 20% of high-value hospital charges that drive 80% of denials impact.