Healthcare organizations are feeling the pain as their top and bottom lines continue to contract. However, despite redoubled efforts, leakage in healthcare revenue cycles continues to impact many organizations at a broad and deep level, exacerbating this financial pressure. To mitigate this, organizations must look across their cycle to identify potential areas of risk.
Stopping Leakage in the Healthcare Revenue Cycle
The healthcare revenue cycle offers ample opportunity for leakage from end to end. Inefficiencies in your organization’s RCM seriously threaten its operational health. In response to this inconvenient truth, healthcare providers are shifting away from manual processing systems to automated, electronic processes.
By examining each stage of the cycle, any sources of leakage that your facility may be experiencing become easier to identify. Though the lines between the three phases of RCM are indistinct, some steps belong squarely to one part of the cycle. However, certain processes serve multiple functions and are likely to occur at different points (eligibility verification, for example).
Let’s look at each of these stages to pinpoint the five aspects of the revenue cycle that are likely responsible for leakage in your organization.
Front End
The front end of the process consists of the tasks performed up until the moment of patient admission. They include:
- Scheduling
- Pre-registration
- Authorization / Pre-certification
- Medical Necessity
- Registration
These initial steps are crucial in your RCM process, as whatever happens on the front end will impact how the back end performs. Receiving complete and accurate information from patients during registration will help ensure a smooth billing and collection process. Conversely, incomplete or inaccurate data is likely to result in denials from insurers, leading to an arduous denial management process on the back end.
The goal of customer satisfaction should be top-of-mind during this phase of the cycle. Patients increasingly see themselves as patrons of the facilities and providers they visit, expecting friendly and engaging service. This makes the front end an even more important part of your revenue cycle, given the correlation between a customer’s satisfaction and the likelihood of retaining them. Optimizing your front-end processes will therefore help ensure a positive patient experience and support your organization’s revenue integrity.
Although room for improvement certainly exists in each of the three overlapping phases of your organization’s revenue cycle, many aspects of the front end can be especially problematic. Many claims denials stem from oversights and errors before a patient visits their provider. The most under-examined parts of the cycle’s front end are pre-registration, authorization (aka pre-certification or prior approval), and eligibility verification.
1. Pre-Registration
Keeping patient collections and payer reimbursements high must begin at the front end of the revenue cycle. Pre-registration is, therefore, the most critical step of RCM. It bridges the gap between scheduling and admission, demanding the utmost accuracy and efficiency for your organization’s revenue integrity. Using this moment to financially clear patients will protect your payer reimbursements, encourage the collection of patient payments, and improve overall patient satisfaction.
2. Authorization
Since payers must confirm whether particular medications or procedures will be approved for patients, providers should contact insurance providers for approval before performing any necessary procedures (preauthorization). Though retroactive authorization may be granted for emergency admissions, some payers deny claims if patients accept medical care without obtaining authorization before treatment. As a result, errors in this step often lead to denials, making it worth your organization’s attention.
3. Eligibility Verification
A patient’s insurance eligibility verification is one aspect that could happen at different stages. This time-consuming process requires advanced knowledge of clinical codes to ensure they’re applied correctly in your claims. Intense workloads and tight deadlines can make the tedious task of verifying insurance coverage a challenge for providers. Consequently, the revenue integrity of your organization calls for a staff that’s been trained in all aspects of eligibility verification to efficiently accomplish this task.
Mid-Cycle
The phase in the process that includes patient access and the activities of your patient accounting/business office, or the mid-revenue cycle, encompasses:
- Clinical documentation
- Case management
- Charge processing
- Clinical coding
Much attention has been given to the front and back ends of the cycle, whether receiving payments upfront or minimizing unpaid accounts receivable in the back office. The importance of an organization’s mid-revenue cycle is only recently being understood and appreciated. Initiatives like Clinical Documentation Improvement (CDI) and training in Computer Assisted Coding (CAC) have become more common as the need to maximize reimbursements has grown.
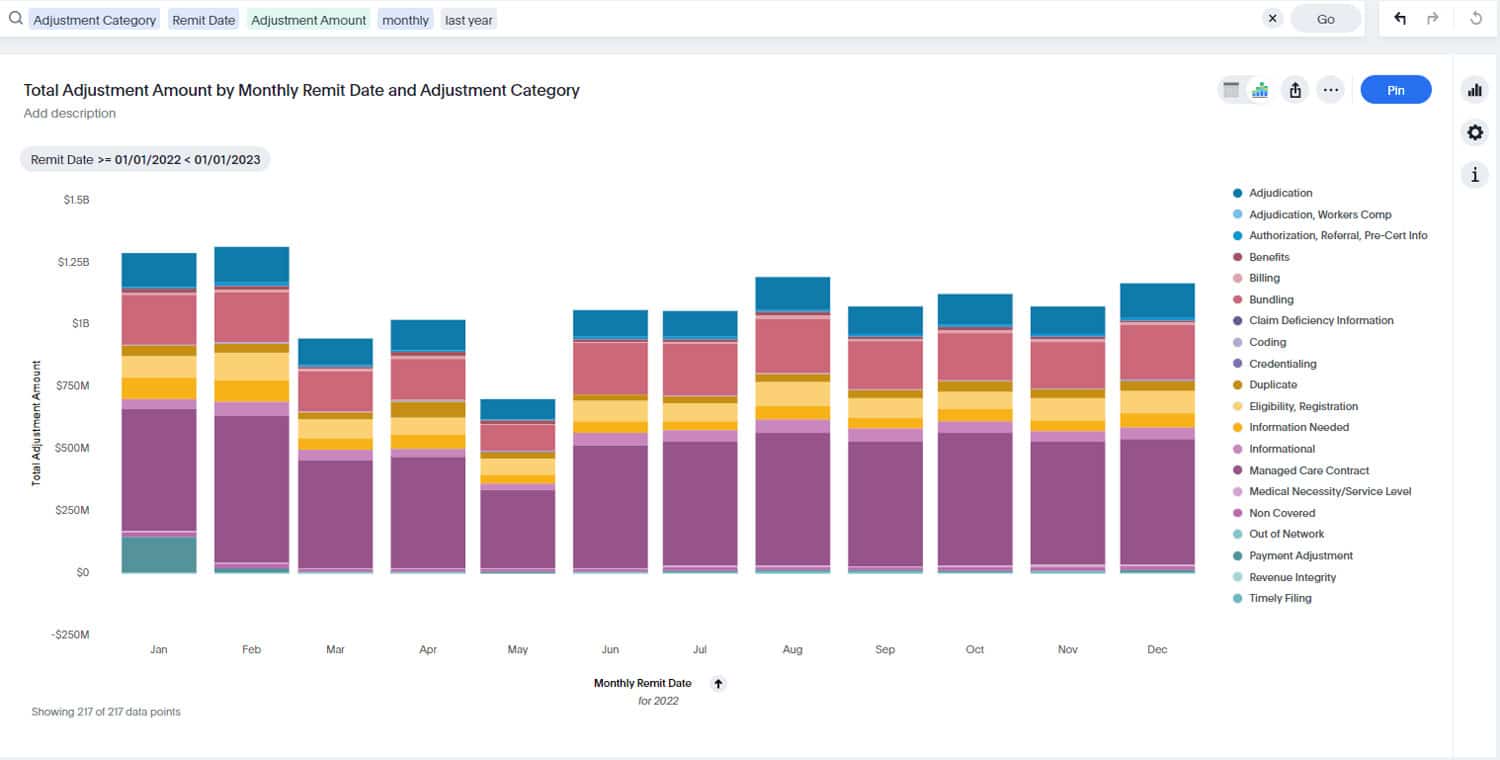
Technology plays a key role at this stage. Purpose-built software solutions can streamline the coding and documentation process to help you detect anomalies and identify billing trends. Moreover, with the publication of ICD-11, new reimbursement models are driving healthcare providers to focus more audit activities on clinical coding. Given the high demand for accuracy and precision within the coding process, paying attention to this stage is crucial for stopping leakage and promoting revenue integrity throughout your organization.
4. Clinical Coding
Coding a patient’s visit properly and complying with payer requirements is a core element of your organization’s revenue integrity. Despite this, many healthcare providers neglect to consider coding as part of the process. Coders often report to a compliance director instead of a revenue manager, which only serves to keep the coding and billing teams siloed. Lack of effective collaboration among these departments is a prime source of revenue leakage. Consider a CAC training program to help optimize your mid-cycle.
Back End
This part of the process comprises all patient accounting services. The steps that take place between patient discharge and final account resolution include:
- Billing
- Collections
- Insurance follow-up
- Cash posting
- Denials management
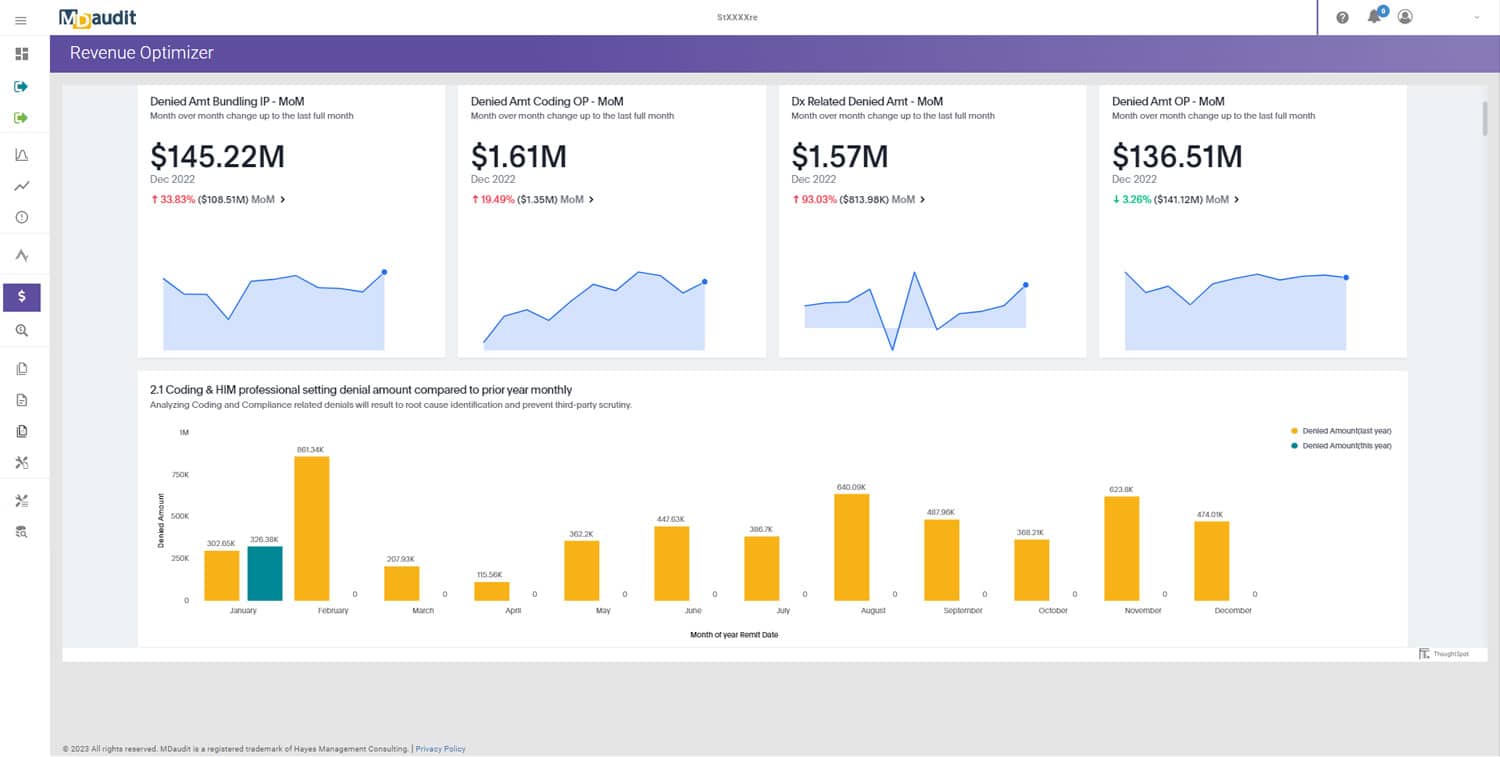
Billing and collections generally pay ample attention to the ongoing effort to plug leaks and reinforce revenue integrity. However, with payer denial rates experiencing all-time highs since the onset of COVID-19, denial management has assumed a more central role in RCM, calling for closer examination. This overlooked part of the revenue cycle is critical for determining root causes of denials to prevent them from happening.
5. Denials Management
With denials accounting for 15–20 percent of the total value of claims and consuming an average of almost three percent of organizations’ annual net revenue, the importance of having a strong, data-driven denials management program for your organization has never been greater. Yet again, technology can mean the difference between success and failure in this area. Automated audit workflows and analytics programs can help you go beyond fixing transactional errors ad hoc so you can implement long-term corrective actions.
An emphasis on the quantity rather than the quality of appeals is partially responsible for the heavy revenue leakage inherent in this aspect of the cycle. Instead of appealing as many denials as possible, your organization should focus on denials prevention by getting to the bottom of each denied claim. Understanding the root causes of denials is your key to increasing first-pass pay rates and decreasing days in accounts receivable. That understanding will help you boost revenue integrity.
A Case for Revenue Integrity
Maximizing your organization’s revenue stream requires more than ensuring each process in the cycle is executed as efficiently as possible. A fundamental flaw in many RCM programs is their failure to align the various departments performing the functions of RCM. As a result of this siloed method, teams often operate reactively to revenue leakage and fix errors on a transactional basis rather than proactively creating long-term solutions.
Revenue integrity programs take traditional RCM steps further by using a holistic model to optimize the cycle. Successful revenue integrity programs achieve three primary goals:
- Departmental alignment that promotes operational efficiency
- Increase in reimbursement collection through better audit processes and improved denials management
- Billing compliance ensured by the elimination of overcoding and undercoding
The results of implementing revenue integrity speak for themselves. Organizations that have established such programs saw their net collection increase by 68 percent, realizing 61 percent overall gross revenue capture and a 61 percent decrease in compliance risk.
Most revenue leakage is avoidable. Your organization can identify and correct the inefficiencies in your organization’s RCM by examining each stage of the lengthy cycle — front end, mid-cycle, and back end — and addressing under-examined aspects such as pre-registration, clinical coding, and denials management. Revenue integrity programs take a holistic approach to RCM to connect your organization’s disparate departments to optimize your revenue cycle.
Contact us to learn more about how MDaudit can help you optimize your revenue cycle.