Why health systems need actionable insights, benchmarking, and data transparency to protect revenue and thrive under rising audit pressure.
Intro
Audits are no longer rare disruptions in healthcare. They are constant, costly, and increasingly complex, leaving systems that aren’t leveraging the right technologies at risk of being left behind. Payers are increasingly applying AI and other technologies to deny more claims, external audits are multiplying, and health systems are under relentless pressure to improve margins while staying on top of compliance. Adding to the challenge, this is all happening while hiring remains a challenge across the healthcare landscape.
Did you know? Medicare RACs recovered over $10 billion in improper payments from 2010 to 2020.¹ And up to 9% of hospital claims face some form of audit.²
- CMS: “Recovery Auditing in Medicare and Medicaid” — cms.gov
- OIG: “Hospital Claim Reviews and Payment Denials” — oig.hhs.gov
In this environment, success depends on more than compliance checkboxes – it requires clear, reliable insights into risk, performance, and outcomes. This visibility is most easily achieved by working with a trusted technology partner offering robust data transparency and actionable insights. Without such a partner, audit teams are left chasing information across spreadsheets and email chains, while executives struggle to understand the true causes and financial impacts of denials and audits.
With help, however, health systems can spot trends earlier, allocate resources wisely, and turn audit management into a strategic function that safeguards revenue and reduces future risk. For too long, audits have been treated as a reactive function. Forward-looking organizations, however, are reframing audit management as an opportunity to gain proactive visibility into risk, revenue, and performance. This shift is made possible by on-demand, up-to-date reporting, benchmarking, and analytics. As part of a leading platform like MDaudit, these capabilities allow health systems to move from putting out fires to planning for the future.
The Rising Stakes of Delayed and Incomplete Visibility
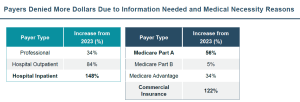
Digging into the numbers yields a clear picture of what health systems are facing in terms of audits and denials. According to MDaudit’s 2024 Benchmark Report, external payer audit volumes more than doubled in 2024, with at-risk dollars increasing nearly 5x year-over-year, jumping from $2.6M to $11.2M per organization. Denials tied to medical necessity and documentation surged as well across professional, hospital outpatient, and inpatient settings, with denied dollars for the latter climbing a massive 148% from 2023 to 2024. This trend held true across both public and private payers as well, most markedly with commercial payers, who denied 122% more dollars in 2024 vs. the year prior.
When reporting and data transparency are limited, health systems often don’t see these risks until the revenue is already lost. Leaders don’t just need audit status updates; they need visibility into financial risk, ROI, and organizational performance. McKinsey, in a report earlier this year, estimated that improving healthcare efficiency and resource allocation through better data use could unlock more than $1 trillion in global economic value while strengthening resiliency. That opportunity depends in part on data transparency and insights that tie operational activity to measurable outcomes. With this in mind, healthcare leaders across the country prioritizing data integration, reporting, and analytics.
Did you know? 90% of healthcare leaders say better reporting and analytics are essential for managing performance.¹ And 78% say data integration and access are key priorities in digital transformation.²
- Deloitte: “The Future of Data Analytics in Healthcare” (2022)
- HIMSS: “2021 Healthcare Leadership Survey” — himss.org
It’s one thing to identify reporting, analytics, and data integration and access as priorities, but what do these elements look like in practice? An ideal technology partner should be able to provide all of these capabilities together, surfacing insights that point leaders to where they need to evaluate and act.
MDaudit is one such partner. By offering health systems a platform that tracks compliance and revenue trends in real time, MDaudit provides immediate visibility into issues like where claims are failing, potential or actual revenue impact, and how quickly staff are responding, among other valuable insights. MDaudit customers, for example, collectively retained more than $250M in revenue tied to payer audits alone in 2024 through transparent audit tracking and tools that enabled proactive intervention.
Data Transparency Drives Informed Action
The MDaudit platform consolidates billing compliance, payer audit management, and revenue integrity workflows into a single cloud-based solution, with transparency built in at every level. We understand that too many leaders don’t have the data necessary to quickly understand the health of their programs, share key trends within their organizations, and drive targeted improvements. On top of the powerful workflows offered by the MDaudit platform, we’ve worked to empower leaders with everything they need for informed decision making.
One example is MDaudit’s new ROI Summary Dashboards, which provide immediate transparency into the essential elements of programmatic performance that matter most. Leaders can easily assess programmatic health and trends over time, from audit coverage to provider performance to risk reduction and revenue retention. In short, ROI Summary Dashboards are your window into the data you need to make decisions and identify needs. Key benefits of this exciting new feature include:
- AI Summaries synthesize key data points from across the entire ROI Summary dashboard into an essential digest to help you know where to dig in.
- The latest data, on demand. No more waiting for manual reports based on stale data.
- Seamless exports of visualizations and underlying data to support presentations and further analysis.
- Support for both internal and payer audit programs
This robust in-platform analytical and reporting capability eliminates the need for third-party tools and empowers leaders with timely, relevant intelligence. Together, these capabilities reflect what the industry urgently needs: real-time visibility, actionable insights, and transparent ROI to strengthen both compliance resilience and financial performance
Benchmarking builds on reporting insights by adding essential context
One final key element worth mentioning when it comes to finding the right partner to bring your data to life is context. Where reporting helps show what is happening in a system, benchmarking further contextualizes insights in the broader audit landscape to help identify strategic priorities. An MGMA survey found that while 84% of medical groups use benchmarking to guide operations, most only do so annually. This leaves leaders making decisions without timely context.
Regular benchmarking transforms reporting from static numbers into actionable intelligence. By embedding benchmarking directly into its platform, MDaudit gives leaders the ability to compare denial trends, audit outcomes, and provider performance not only internally but against industry peers. As Becker’s Healthcare noted in 2024, “by analyzing their own reimbursement data alongside benchmarking data, providers can streamline revenue cycles, improve profitability, and reduce re-work.” In short, benchmarking ensures reports don’t just inform but go a step further to help direct action.
Final Thoughts
Audit management has reached a tipping point and reacting is no longer enough. Forward-thinking health systems are leveraging robust, transparent reporting, innovative analytics, targeted AI, and more frequent benchmarking as part of their toolkit to go beyond merely surviving payer scrutiny to thriving financially. With clear, accessible, contextualized reporting, executives and audit managers alike can move beyond reacting to audits and instead use them as a lens for identifying risk, improving processes, and protecting margins.
Platforms like MDaudit show what’s possible when transparency becomes the standard: faster decisions, stronger compliance, and better financial outcomes. In a healthcare landscape defined by rising audit pressure, data used correctly isn’t just an operational tool—it’s a strategic advantage.